CRS/HIPEC Shows Long-Term Survival Benefit for Advanced Ovarian Cancer (OVHIPEC-1)
- Aug 15, 2025
- 2 min read
S Lot Aronson, Marta Lopez-Yurda, Simone N Koole, Prof Jules H Schagen van Leeuwen, Hendrik W R Schreuder, Ralph H M Hermans, et al.
Cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy in patients with advanced ovarian cancer (OVHIPEC-1): final survival analysis of a randomised, controlled, phase 3 trial. The Lancet Oncology 24, (2023) 1109-1118.
Summary:
A major clinical trial from the Netherlands, OVHIPEC-1 followed women with stage III epithelial ovarian cancer for 10 years and found that adding HIPEC to cytoreductive surgery helped patients live longer and delayed the return of their cancer compared with surgery alone. All patients first received standard chemotherapy before surgery, and those who received HIPEC lived a median of 45 months, versus 33 months for those who did not, with no increase in serious side effects. The study confirms that for women with advanced ovarian cancer, combining HIPEC with cytoreductive surgery can provide a meaningful, long-term survival benefit while maintaining quality of life.
Background
Researchers wanted to see if adding HIPEC (Hyperthermic Intraperitoneal Chemotherapy) to cytoreductive surgery could help women with advanced stage III ovarian cancer live longer and delay recurrence compared to surgery alone.
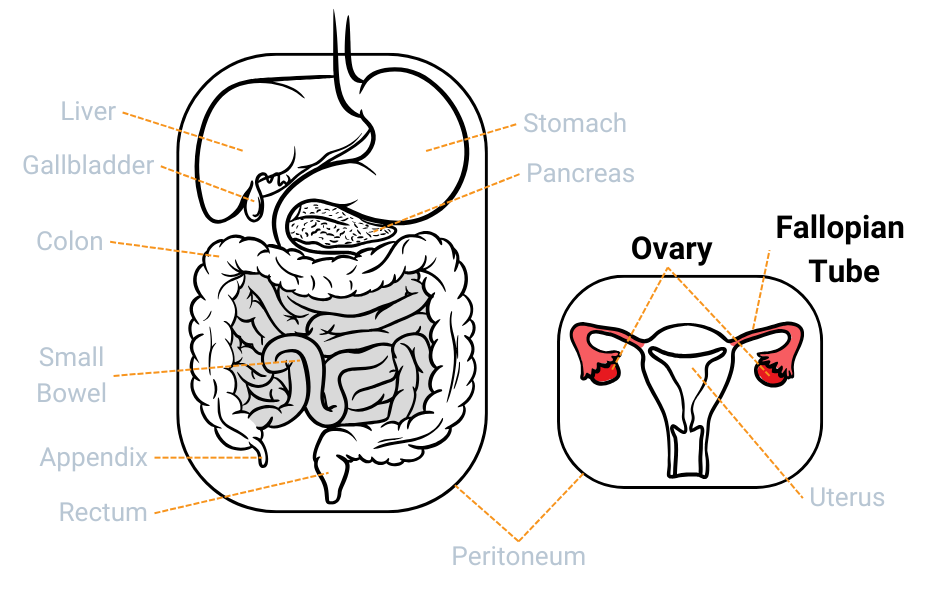
HIPEC is a treatment in which heated chemotherapy is circulated directly into the abdomen following cytoreductive surgery to kill any remaining microscopic cancer cells. This allows the medicine to reach areas regular systemic, or intravenous, chemotherapy might miss.
What Was Done
Researchers studied 245 women with stage III epithelial ovarian cancer. All patients received systemic chemotherapy before surgery (also called neoadjuvant chemotherapy). During surgery, half received cytoreductive surgery alone, and half received cytoreductive surgery plus HIPEC with the chemotherapy drug cisplatin. Participants in this study were followed for 10 years.
What They Found in OVHIPEC-1
Cancer took longer to come back in the HIPEC group (about 14 months) compared to those who had surgery alone (about 11 months).
Women who received HIPEC lived longer overall: a median of 45 months, compared to 33 months for surgery alone.
After five years, about 37% of women who received HIPEC were still alive, compared to 20% who had surgery alone. After ten years, the difference persisted (16% vs 11%).
Side effects and recovery were similar in both groups.
Why It Matters for Patients
This long-term follow-up confirms that HIPEC provides a real, lasting survival benefit for patients with advanced ovarian cancer who are not eligible for primary debulking surgery. Importantly: the benefit wasn’t due to differences in treatments after recurrence; fewer HIPEC patients developed platinum-resistant disease, meaning they were more likely to respond to future chemotherapy; and quality of life was preserved after treatment.
Bottom Line
This study shows that adding HIPEC to complete cytoreductive surgery can improve both survival and quality of life for some patients with advanced ovarian cancer. HIPEC may also help reduce the chance that the cancer becomes resistant to chemotherapy later on. Every case is unique, so it’s important to discuss options with your care team.



